There must be someone who reads Brownstone Journal who is a fan of the television show Monk, as I am. I sing along with the theme song, “It’s a jungle out there,” written by Randy Newman. When in the song I get to Monk’s great tag-line, “I could be wrong now, but I don’t think so,” my volume and expressiveness make my wife wince. Those just seem like great words to live by…if you occasionally back them up with results.
It’s fun to be right, but there can be a dark side to being right.
In Brownstone writings, I’ve documented and predicted a few outcomes of the travesties and tragedies forced on the public by politicians and public health officials during the Covid lockdown years; public health officials who, in title, anyway, are responsible to guard and to improve public health rather than selectively impair or destroy aspects of the health of the public. We expect politicians to be malignant influences – not so much public health officials. Or, maybe that’s what we once thought.
As background for how predictions can be made, let me briefly describe a few things about how vision works – vision is what I work in and research. Vision and its neurology are described in a little more detail here and here.
In a nutshell, visual neurology and therefore visual abilities develop from the eye up to the brain. The brain actually calculates what you see. Your entire visual world is about 10 milliseconds behind reality – brain calculation time. Vision is something like 80% of the sensory input to the brain. Therefore, making vision somehow less patent is literally limiting information input to the brain.
The foundation upon which your visual world is built is visual motion and its detection by the visual neurology. One specific set of visual neurology (called a pathway) carries “regular motion” to the brain, and without that motion detection, you don’t see. Literally, the neurology goes into sleep mode just like a computer. That dropout of vision likely occurs at a relay station about halfway up to the brain, which reduces sensory input to the brain.
A separate neurological pathway carries visual detail and color, and it is this pathway that goes to sleep when visual motion isn’t at threshold levels. A third pathway carries “surprise” very fast motion. This third pathway goes by a separate route more directly up to the area of the brain that processes motion, the middle temporal area. This neurological setup has real significance in different health, trauma, and developmental conditions. For example, when the “regular motion” pathway is impaired, if the separate route of that third “surprise” pathway is unimpaired, now that person has much greater input by “surprise” versus “regular” motion. That may explain some of the motion sensitivity that people can have when in other ways their two-eyed binocular vision is defective, so not getting regular motion to the brain intact.
As I and others and I started to figure all this out, I made some predictions about Alzheimer’s disease. In Alzheimer’s, that “regular motion” pathway is selectively injured. That means the detail and color pathway isn’t supported, so sporadically “goes to sleep.” It was a logical extension to suggest that, as the detailed visual signal to the brain gets less stable with Alzheimer’s damage, face detection might be impaired.
Trying to feel out if that prediction had any merit, I started asking people with family members afflicted with Alzheimer’s if that family member recognized them a little more easily if they spoke to their Alzheimer’s family member, and the answer frequently was “yes.” In 2002, I published my prediction of face detection problems in Alzheimer’s and that was confirmed in 2016 in very separate research. Covid lockdowns in my town separated people with Alzheimer’s cognitive issues from their loved ones when that Alzheimer’s patient was in a separate memory care unit. Visitation was not allowed. This was a tragic if not malevolent treatment of these people, afflicted with a terminal disease. The paper published in Brownstone Journal includes a case study.
At the 2-year lockdown mark (2022), Brownstone Journal published the results of a worldwide survey study I was involved with, asking the question whether nearsightedness (myopia) was increasing in frequency during the Covid lockdown years. Myopia is marginally less complex to understand than how a visual signal makes its way to the visual cortex using the neurology outlined above. The myopia research suggests near work, such as staring at a screen, creates an out-of-focus ring around the central vision that triggers some chemical changes allowing the internal eye pressure to lengthen the eye – especially when favored by the individual’s genetics.
Our international survey study results said yes, we think we’re seeing more myopia and faster increases in myopia. That was recently confirmed by a late 2024 study published in the British Journal of Ophthalmology. Ours was a survey, theirs was data. In fairness, ours was probably earlier than real data could have been developed and accumulated. In our study we had optometrists in 32 countries suggesting that myopia during the lockdown years had increased its prevalence and pace. Broadly increasing myopia rates have wide consequences since other eye problems, such as retinal detachment, have a higher incidence in myopic eyes. The British Journal data agreed with our survey.
What I didn’t see coming was a spike in astigmatism.
Are you wondering precisely what astigmatism is? Most normal people do wonder about this weird word. As an imperfect description, first, imagine the front of the eye. The clear dome that you look through is called the cornea, and the cornea is where the vast majority of the “work” of focusing light on the back of the eye, the retina, occurs. The amount of focusing is a function of the curvature of the cornea. You can have laser surgery on the cornea for nearsightedness because the change in curvature has a big effect on the focus at the retina.
With no astigmatism, that clear corneal dome has a fairly regular curvature in the center. It’s “round” if you will. Now, imagine instead of looking at a round, smooth cornea, you’re looking at a Pringles potato chip. If you hold the Pringles potato chip so you can look side to side along the length of it, it has some curvature, but not a lot. If you then turn the Pringles potato chip 90 degrees so you’re looking at the end of it, it has a much sharper, much more drastic curvature. That’s astigmatism. The front of the eye, the cornea, has two different curvatures. If that’s the front of your eye, you can imagine one of the forces involved could be eyelids pushing down on the long sides of the chip.
We think we’re starting to understand how myopia develops, and therefore when we stick kids inside looking at screens all day long without some glasses to relieve the strain, it’s not a big surprise when someone starts into nearsightedness. We have a lot less convincing science about how astigmatism develops. Genetics come into play with both myopia and astigmatism. Genetics was my first thought when I had a teacher from a small outlying town come to my office. She told me incoming first-graders couldn’t see because of astigmatism. Some groups do have higher levels of astigmatism, so we often think genetics is the culprit for high levels of astigmatism. Just a little discussion swerved my thoughts away from genetics. It sounded like a local plague.
That elementary school teacher told me she could pick out the kids whose parents just left them in front of screens for school during lockdowns (and probably for video games), and those were the kids who came into school with large amounts of astigmatism. As I continued to ponder that, after the teacher’s visit, I had a nine-year-old girl come into my office with a lot of astigmatism. She was also squinting; squinting so hard that her eyelids were curling in and her lashes were poking the fronts of her eyes, poking her corneas. Kids are a significant part of my practice, but I hadn’t seen that one before. Her eyelids were literally pushing hard on the top and bottom of the Pringles potato chip.
Which came first, the astigmatism or the squinting? In this case, it doesn’t much matter. She needs to see and to not squint so she doesn’t deform her corneas more. Genetics could easily come into play in setting the stage. Genetically determined relatively softer corneal tissue might deform more easily than genetically determined stiff tissue.
I’ve seen kids, and occasionally adults, who squint hard, who over time seem to make their astigmatism worse. I’ve gotten to the point that I tell kids pretty firmly “DON’T SQUINT!” I do smile and say it in fun ways. But, squinting to alleviate in some way the eyestrain of looking at screens all day for your schooling might explain the lockdown-period astigmatism increases. Squinting has the optical effect of reducing the effective aperture for light to come through and so the depth of focus increases. The price for this behavior includes making other people wonder why you look like that, as well as potentially increasing astigmatism.
Those changes in astigmatism aren’t just a local phenomenon here. A recent study published online in JAMA Ophthalmology documents a 20% increase in astigmatism in Hong Kong, with the blame laid on lockdowns. The increases are in “both prevalence and severity” of astigmatism. They provide no scientific or physiological mechanism for this broad-based development of significant astigmatism. Maybe someone has a physiological theory alternative to squinting. Certainly, early unilateral astigmatism seems congenital, with some genetics involved, and is part of lazy eye – amblyopia. But this science blamed lockdowns (it does avoid the term “cause”) and the stress of screens – without further suggestion of mechanism.
To this point in this Brownstone Journal literature review, we’ve looked at how we’ve frightened the elderly who have Alzheimer’s and driven the eyes of children to develop myopia and astigmatism beyond prior typical amounts. Directly attributable to lockdowns.
Perhaps the scariest prediction of possible damage to children came from my study of how face detection develops in children. I hadn’t really thought about face discrimination since learning in college that the brain has a specific area dedicated to recognizing faces. But, early in the Covid mask era, I had someone in my office who worked in a daycare that included infants, and she told me how all the adults were masked up in the daycare. That sent me down the trail of wondering if we might be messing with how specific visual neurology related to face discrimination developed.
The research I found showed that if the development of face detection neurology has interference, especially in the first six months of life, whatever deficit that occurred is not repairable. Further, if face recognition were impaired, it made neurological sense that fear may play a bigger role in responses to the faces of others.
I hypothesized that if surrounding infants with people in masks interfered with the development of face detection in those infants, then impaired ability or desire to respond to faces might be considered a sign of autism. If there were any validity to that prediction, then we would expect to see an increase in autism diagnoses at very young ages relative to older groups. Autism diagnoses overall might be increasing because of testing changes, or other exogenous factors, including vaccines.
But, since face detection changes selectively affect younger versus older groups (excluding specific brain trauma), those other factors would likely affect similar age groups equally, increasing their diagnosis rates equally. That could leave something like impaired face detection as a likely suspect for age-group differences. If autism diagnosis rates are accelerating, then data showing accelerating rates of diagnosis year-to-year should show greater acceleration in younger versus older age groups.
A late 2024 JAMA Network open access study by Grosvenor, et al looked at the changes in autism diagnosis from 2011 to 2022 and as part of their data analysis, they separated out age groups. They also provided their data tables as a courtesy to those who might want to look further into the subject. The data comes from a cross-sectional study of electronic US health and insurance claims records for over 9 million individuals per year from 2011 to 2022 in a multi-center health system.
Below are their graphs of that data that require some analysis of the associated numbers. The authors don’t comment on why these changes occurred. They instead concentrate on documenting the changes in diagnosis rates since autism diagnoses seem to be increasing across all age groups. The question then is whether the younger groups are different in a – perhaps – predictable way. In my analysis, I concentrated on the four, and sometimes five, youngest groups. It’s important to understand that the data points are limited – it’s only been five years, and data for more recent years has to be collected, analyzed, and written up – that takes time.
A cursory examination of their graph suggests younger groups are diagnosed at higher rates than older groups. But also, there seems to be an inflection point about the year 2020.
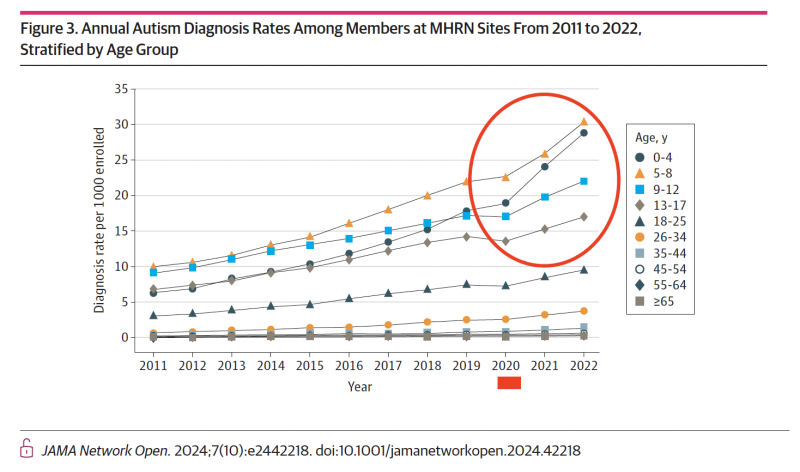
That inflection point leads to a noticeable change in the acceleration of diagnostic pace for younger groups. The authors only address that by saying 2020 rates were probably lower because of lockdowns. If true, we might expect a jump up in 2021, but not necessarily a continuously higher and accelerating rate of diagnosis beyond that time. A more mathematical way of saying that is we might expect the slopes of the diagnosis rate lines would be similar before and after a pause around 2020. Notice that some diagnosis rates did decrease a little in 2020, but they didn’t go to zero.
If we interfered with face recognition development by surrounding infants with people in masks, and if loss of face recognition is interpreted (or defines) an autism diagnosis, then we would expect younger kids to be most affected. The youngest would probably be affected the most, but we might see some effect in toddlers since there may still be some neural development we interfere with after infancy. As in most timetables of neural development, our information is incomplete and confounded to some degree by individual variations.
The Grosvenor, et al data can be tortured to the point it will bleed many things, but such torture can obscure the basics. Maybe the easiest way to suggest there may be something in this data is to say that if you were part of the study group and were in the 18-to-25-year-old group, prior to 2020 your group was seeing pretty steady increases of diagnoses of autism of 0.56 diagnoses per 1,000 health system enrollees per year. If we remove the 2020 data point as an anomaly, the pace of increase in diagnoses increases…to 0.58 additional diagnoses per 1,000 enrollees per year.
So, the general curve of diagnoses of autism is sloping up to more and more diagnoses. The rate of diagnosis is increasing year-to-year, not just the raw numbers of people diagnosed. If we include the 2020 inflection point, which was a “down” year for the 18-to-25 group in a slope calculation starting in 2020, the slope does increase to 1.1 more diagnoses per 1000 per year, or almost twice the rate of increase as prior to 2020.
If we look at the 0 to 4-year-old group, the data show a different story. Prior to 2020, the diagnostic rate was increasing at 1.40 diagnoses per 1,000 health system enrollees per year. So, the rate is definitely increasing. From 2020 on, that rate of increase is now 4.95 diagnoses per 1,000 health system enrollees per year, and 2020 was not a down year for infant autism diagnoses.
Here’s where care is needed in evaluating the data, and a statistician could tell you much more about this than I can. Further, a good statistician can probably claim foul at some of my analysis. However, just looking at those raw numbers of change, the acceleration in autism diagnoses in the 0-to-4-year-old group is something like three-and-a-half times as fast as it was prior to Covid lockdowns. Older groups don’t show the same magnitude of acceleration, and if the year 2020 is dropped out in groups as a year in which diagnoses became more rare rather than more common, the inflection point can basically disappear.
I don’t know how we can tell if this is from inhibiting development of face detection neurology. So many things were wrong about lockdowns that other factors can certainly be part of the picture. However, mine was a fairly specific worry about increasing diagnoses of autism, specifically in the youngest groups. Unfortunately, I may have been right. This is the dark side of being right.
So, what do we do?
First, of course, is that we don’t let this happen again.
Next is on my professional level; and that is, as I alerted the Asia Optometric Congress to last November in a Zoom lecture, we – eye care and other medical people – need to pay attention and if a child is in our office who fits this description, we need to do – or refer for – specific current therapies to address as many vision and binocularity issues as we can and then report any successes to the world at large.
Last – and this is a pipe-dream – every local, regional, state, and national public health official who went along with lockdowns and therefore is dangerously unfamiliar with the term, “unintended consequences,” needs to resign, be fired, and potentially have charges brought against them since it now looks verifiable that they have through malfeasance, negligence, and incompetence injured a generation of children.
I could be wrong…but I don’t think so. It’s a jungle out there.
BREAKING: Sources Confirm To Alex Jones What Infowars Reported A Month Ago: Trump Is COMPLETELY DONE With Netanyahu!